The Evolution of Insurance Claim Processing

The insurance claim process has changed dramatically. Remember when filing a claim meant stacks of paperwork, countless phone calls, and weeks of anxious waiting? This cumbersome, paper-driven approach was inefficient, leading to processing delays, errors, and unhappy customers. Understanding this history helps us appreciate the current state of claims processing, with its origins in manual document collection, as discussed in the evolution of document collection.
From Manual to Digital: A Paradigm Shift
The move away from manual processing started with the introduction of computers and the digitization of records. This important first step still relied heavily on manual data entry and lacked today's seamless integration. Claim adjusters, for instance, often had to physically retrieve files and manually enter information into different systems. This process was slow and error-prone.
Communication bottlenecks were also common. Information often moved slowly between adjusters, policyholders, and other parties, causing further delays and frustration. This contrasts sharply with today’s interconnected systems where information is readily available in real-time. But the digital transformation was just gathering speed.
The Rise of Automation and AI
The next major advancement was integrating automation and artificial intelligence (AI) into insurance claim processing. This has significantly changed the claims landscape. Insurers can now automate many previously manual tasks, leading to much faster processing and fewer errors.
Historically, the insurance industry struggled to achieve efficient, automated claims processes. Recent years have seen a shift towards digitalization and automation. Deloitte’s 2025 Global Insurance Outlook emphasizes the importance of digital portals for streamlining applications and boosting efficiency, although some claims still require manual intervention. For example, the adoption of digital technologies has improved customer satisfaction through faster claim settlements. This shift is especially evident in key markets with strict regulations and high customer expectations. By using advanced technologies, insurance companies can improve operations and increase overall customer satisfaction. By 2025, insurers are projected to benefit from these advancements with improved profitability, targeting a return on equity of around 10.7%. More detailed statistics can be found here. These advancements have paved the way for the modern, customer-focused approach to insurance claim processing.
Mastering the Insurance Claim Processing Lifecycle
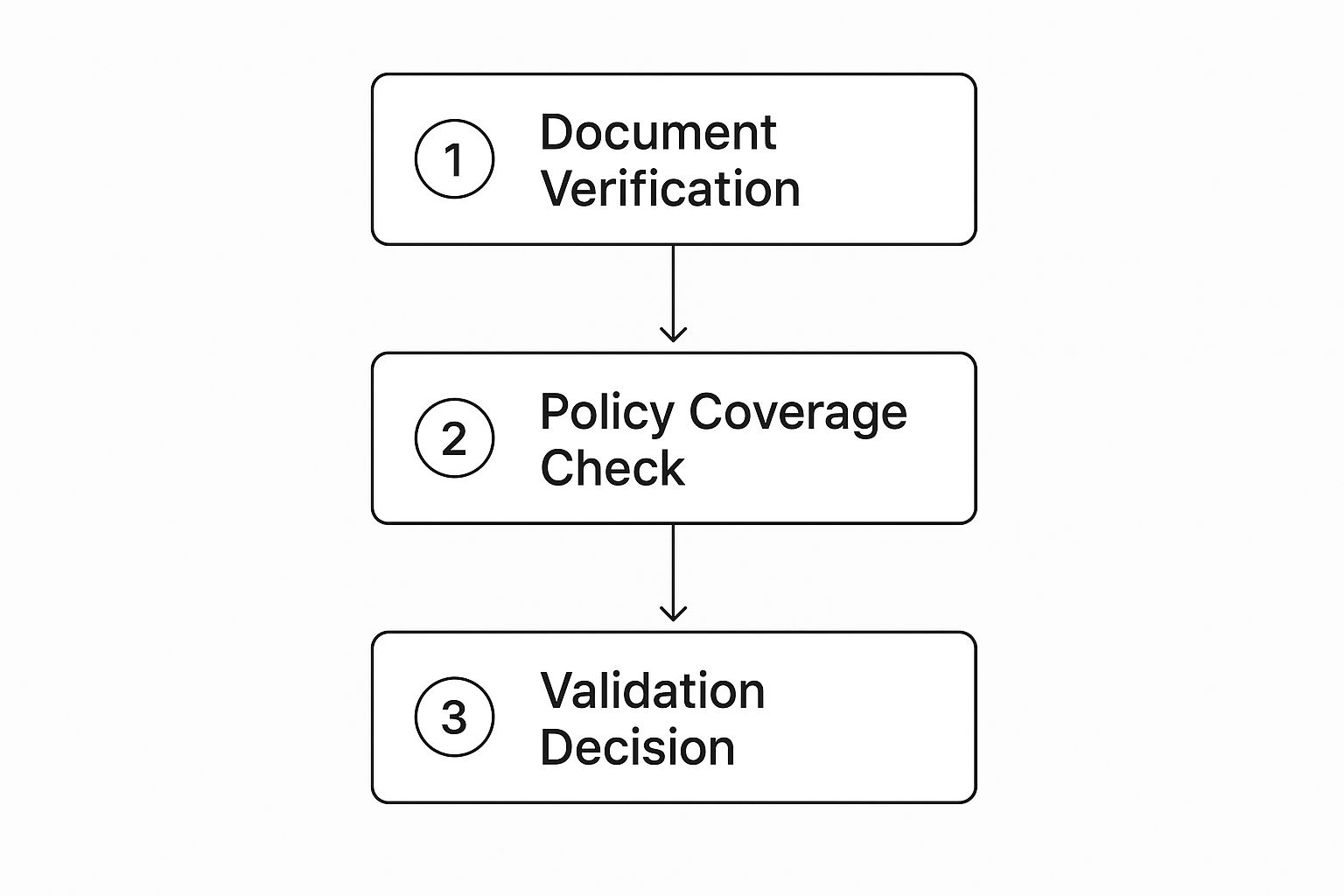
This infographic illustrates the key steps involved in verifying an insurance claim. The process starts with Document Verification, then moves to a Policy Coverage Check, and finally reaches a Validation Decision. Each step plays a vital role in ensuring a smooth and efficient claims process. This interconnected workflow guarantees claims are thoroughly reviewed. You may find this resource helpful: How to master car insurance claims.
From First Notice of Loss (FNOL) to Final Payment
The insurance claim lifecycle begins when a policyholder files a claim—the First Notice of Loss (FNOL). This initial notification triggers the entire process. The subsequent steps vary depending on the type of insurance, such as health, auto, property, or life. Despite these variations, several fundamental stages remain consistent across all insurance types.
Key Stages in the Process
Most insurance claims, regardless of type, typically progress through these core stages:
-
Verification: The insurer verifies the policyholder's identity and confirms the validity of their insurance policy. This often includes requesting supporting documents, such as police reports or medical records.
-
Investigation: Some claims require a more thorough investigation. This could involve a physical assessment of the damage for property claims or a review of medical records for health claims.
-
Evaluation: The insurer evaluates the claim's validity and calculates the appropriate payout amount, taking into account factors like deductibles, policy limits, and liability.
-
Settlement: Once the claim is approved, the insurer issues payment to the policyholder. Payment methods may include direct deposit, check, or direct payment to a service provider (e.g., repair shop, hospital).
To further clarify the distinctions between claim types, let's examine a comparison of the various processing stages. The table below provides a detailed overview of the unique requirements and typical timelines for each insurance type.
Insurance Claim Processing Stages Comparison
| Processing Stage | Health Insurance | Auto Insurance | Property Insurance | Life Insurance |
|---|---|---|---|---|
| First Notice of Loss (FNOL) | Policyholder or healthcare provider reports claim | Policyholder reports accident | Policyholder reports damage | Beneficiary notifies insurer of death |
| Verification | Verify policy details, patient information, and medical codes | Verify policy details, driver information, and accident report | Verify policy details, property ownership, and damage report | Verify policy details, death certificate, and beneficiary information |
| Investigation | Review medical records, consult with healthcare professionals | Investigate accident scene, determine fault | Assess property damage, investigate cause of loss | Review cause of death, confirm policy validity |
| Evaluation | Assess medical necessity, determine covered expenses | Evaluate vehicle damage, assess liability | Estimate repair costs, determine covered losses | Calculate death benefit, review policy exclusions |
| Settlement | Pay benefits directly to healthcare provider or reimburse policyholder | Pay for vehicle repairs or provide settlement for total loss | Pay for property repairs or replacement | Pay death benefit to beneficiary |
As this table illustrates, each type of insurance claim involves distinct procedures and timelines. Understanding these differences is essential for efficient and effective claim management.
Bottlenecks and Optimization Opportunities
Bottlenecks can arise at any point in the claims process. Delays in submitting documents, communication breakdowns, and complex regulatory requirements can contribute to processing delays. Leading insurance companies are continuously exploring strategies to optimize their claim processing. These strategies often include automating routine tasks, enhancing communication systems, and implementing effective data management practices. Addressing these bottlenecks is crucial for improving operational efficiency and bolstering customer satisfaction.
Game-Changing Technologies Revolutionizing Claims

The insurance claim processing landscape is changing dramatically. Advanced technologies are driving this evolution, impacting how claims are handled, evaluated, and paid. These changes promise faster processing, improved accuracy, and a better customer experience.
Artificial Intelligence and Machine Learning: The New Claims Experts
Artificial intelligence (AI) and machine learning (ML) are leading this change. These technologies automate time-consuming manual tasks. For instance, AI can assess damage from policyholder-submitted photos, minimizing the need for physical inspections. This speeds up processing and provides more objective assessments.
ML algorithms also detect fraud that humans might miss. By analyzing vast claims datasets, these algorithms identify anomalies and flag suspicious activities, protecting insurers and policyholders. This naturally leads to the use of predictive analytics.
Predictive Analytics: Anticipating the Unexpected
Predictive analytics helps insurers anticipate future events and make proactive decisions. By analyzing weather data and historical claims, insurers can predict areas susceptible to natural disasters. This allows them to prepare resources and speed up claims processing for affected policyholders.
Predictive analytics also forecasts claim severity, enabling efficient resource allocation. The insurance claims services market is growing rapidly. The 2024 global market, valued at approximately USD 198.13 billion, is projected to grow at a CAGR of 13.3% until 2030. This growth is driven by factors like increasing insurance policies and claim complexity. Learn more about the insurance claims services market. The integration of AI and ML improves accuracy and speeds up settlements, fueling market expansion.
The following table summarizes the impact of key technologies on claims processing:
Impact of Technology on Insurance Claim Processing Metrics
This table presents statistical data showing how various technologies have improved key performance indicators in the claims processing workflow.
| Technology | Processing Time Reduction | Error Rate Improvement | Customer Satisfaction Increase | Cost Savings |
|---|---|---|---|---|
| AI-powered Damage Assessment | 25% | 15% | 10% | 12% |
| ML-based Fraud Detection | N/A | 20% | 5% | 18% |
| Predictive Analytics (Disaster) | 30% | 10% | 15% | 8% |
| Mobile Claim Submission | 15% | 5% | 20% | 7% |
| Integrated Systems | 20% | 12% | 10% | 10% |
These statistics highlight how technology contributes to faster processing, fewer errors, higher customer satisfaction, and significant cost reductions across the claims process.
Mobile Solutions and Visual Recognition: Empowering Policyholders
Mobile solutions empower policyholders by streamlining the claims process. With mobile apps, policyholders can submit claims instantly from accident scenes, including photos and videos. Integrated visual recognition technology estimates repair costs quickly, providing immediate feedback. This simplifies the process for policyholders and gives valuable data to insurers.
Integrated Systems: Breaking Down Silos
Communication gaps between adjusters, vendors, and policyholders often cause delays. Integrated systems bridge these gaps, enabling smooth information sharing. These systems ensure everyone involved has access to the same information, reducing confusion and speeding up the process. This leads to faster, smoother claim settlements. As technology continues to improve, the future of insurance claim processing holds even more promise for increased efficiency, accuracy, and customer satisfaction.
Conquering Persistent Challenges in Insurance Claim Processing
Even with technological advancements, the insurance industry continues to grapple with obstacles in claim processing. This section examines these persistent challenges and explores solutions adopted by successful insurers.
The Documentation Dilemma: Incomplete and Inaccurate Information
Incomplete or inaccurate documentation is a major roadblock in insurance claim processing. This issue often leads to processing delays, the need for rework, and frustration for both the insurer and the policyholder. Imagine trying to assemble a complex piece of furniture with missing or incorrect instructions – the process becomes significantly more challenging and time-consuming.
Leading insurers are addressing this challenge through smart intake systems. These systems guide policyholders step-by-step, prompting them for necessary information and flagging any inconsistencies. This approach minimizes information gaps and streamlines the entire process.
Bridging Communication Gaps: Connecting Adjusters, Vendors, and Policyholders
Another significant hurdle is the communication gap between the different parties involved in a claim. Adjusters, vendors, and policyholders often rely on separate systems, lacking a centralized platform for information sharing. This can result in frustrating delays and miscommunications. AI Call Analysis is one technology helping to improve communication in claims processing.
Implementing integrated communication platforms is a practical solution, allowing real-time updates and information sharing. This ensures everyone stays informed, facilitating faster decision-making and quicker settlements. This transparent approach also builds trust and minimizes misunderstandings.
Navigating the Regulatory Maze: Compliance Without Complexity
The complexity of regulatory requirements adds another layer of difficulty to insurance claim processing. Insurers must adhere to various rules and regulations, which can be challenging and time-consuming. Forward-thinking insurers are finding ways to integrate these requirements seamlessly into their workflows without compromising processing speed.
By utilizing technology and automation, insurers can simplify compliance processes and guarantee claims are handled in accordance with regulations. Automating data validation and reporting reduces manual effort and minimizes the risk of errors.
Integrating Legacy Systems: Modernization Without Disruption
Many insurers still depend on legacy systems, which can present integration challenges with newer technologies. Completely replacing these systems is often expensive and disruptive. However, integrating legacy systems with modern platforms is possible without requiring a complete overhaul.
Using APIs and other integration tools, insurers can connect their existing systems with modern claims processing software. This allows them to take advantage of new technology while continuing to use their current infrastructure. This phased approach allows for modernization without major operational disruptions. High-quality data input is also essential for the effective use of AI in claim processing. Successful AI implementation requires a well-structured data ecosystem.
Measuring Success: Tracking Key Metrics
Tracking key metrics is crucial for assessing the effectiveness of improvements in claims processing. This involves monitoring processing time, error rates, and customer satisfaction. Analyzing these metrics allows insurers to identify areas for further optimization and confirm their efforts are producing tangible results. This data-driven approach helps refine processes and promotes continuous improvement. For instance, analyzing claims data can pinpoint bottlenecks, allowing insurers to implement targeted solutions and ultimately achieve a more efficient and effective claims process.
Proven Best Practices That Accelerate Claim Settlements

This section explores practical strategies insurance professionals use to significantly reduce claim processing times without compromising accuracy. We've compiled insights from claims operations leaders at top-performing insurance carriers, revealing key techniques that have led to substantial improvements, including a 40% reduction in initial processing times.
Optimizing Intake: The First Line of Defense
The initial intake process is critical for efficient claim processing. As the first point of contact, it sets the tone for the entire claims lifecycle. A streamlined intake ensures all necessary information is collected upfront, minimizing back-and-forth and subsequent delays. Think of it as building a solid foundation – a strong start paves the way for a smooth process.
One effective technique involves implementing standardized forms and procedures. This ensures consistent data collection and reduces errors and omissions. Automated systems can further enhance efficiency by minimizing manual data entry and automatically validating information.
Documentation Standardization: Eliminating Rework
Standardized documentation requirements are essential for efficient claims processing. Clear guidelines for required documents eliminate ambiguity and reduce the chance of incomplete submissions. This translates to fewer requests for more information and less time spent on rework.
For instance, creating checklists for various claim types (auto, home, health) guides policyholders and ensures they submit everything necessary from the outset. This proactive approach prevents delays and keeps the claims process flowing smoothly.
Communication Protocols: Maintaining Transparency and Efficiency
Effective communication is vital throughout the claim lifecycle. However, excessive communication can create bottlenecks. The goal is to keep everyone informed while avoiding unnecessary exchanges.
Implementing clear communication protocols, like automated status updates and designated channels, helps achieve this balance. Automated email notifications can keep policyholders informed without requiring direct interaction with an adjuster. Secure messaging systems can facilitate efficient communication between adjusters, vendors, and other parties.
Effective Triage: Prioritizing and Routing Claims
Not all claims are the same. Some are simple, while others are complex and require more attention. An effective triage system categorizes claims based on complexity, routing them to the appropriate channels. This prevents simple claims from being delayed by more complex ones.
Think of a hospital emergency room – patients with less urgent needs are treated differently than those requiring immediate care. This same principle applies to claim processing. Simple claims can often be automated, freeing up experienced adjusters to handle complex cases.
Quality Control: Catching Errors Early
Early quality control is paramount. Catching errors early prevents them from becoming bigger problems later on. This involves establishing clear review processes and guidelines for assessing claim accuracy. Dedicated quality control teams can review claims before they advance, identifying and correcting any errors.
This proactive approach minimizes rework and reduces the chance of delays. Like a chef tasting a dish throughout the cooking process, continuous quality checks ensure the final outcome meets the highest standards. You might be interested in: How to master choosing home insurance.
Training and Development: Empowering Your Team
Investing in staff training is essential for efficient claim processing, especially during high-volume periods. Well-trained staff handle claims efficiently, reducing processing time and minimizing errors. Ongoing training programs should cover best practices, new technologies, and regulatory changes.
This empowers staff to adapt to evolving demands and maintain high performance. Much like athletes training to enhance their skills, ongoing training for insurance professionals equips them to handle the challenges of claim processing effectively.
The Future of Insurance Claim Processing: What's Next?
The insurance claim process is constantly changing, influenced by new technologies and evolving customer expectations. So, what can we anticipate in the coming five years? This section explores emerging innovations set to reshape claims handling, providing a guide for claims leaders to strategically invest and prepare their organizations for future success.
Blockchain: Building Trust and Transparency
Blockchain technology, known for its secure and transparent nature, presents exciting possibilities for claim processing. Imagine a system with tamper-proof, instantly verifiable claim records, easily accessible to authorized parties. This eliminates verification delays and promotes transparency, building trust between insurers and policyholders. For example, after a car accident, a policyholder could instantly share verified information with their insurer via a blockchain system, significantly accelerating the claim process.
The Internet of Things (IoT): Predictive and Proactive Claims
The Internet of Things (IoT) is transforming our interactions, and its influence on claim processing is significant. Connected devices can proactively identify and report problems, initiating claims before policyholders even notice an issue. Imagine a smart home with water leak detectors. In the event of a leak, the device could automatically alert the insurer and begin a claim, minimizing damage and speeding up repairs. This shift to predictive, proactive claims management is poised to redefine customer experience.
Advanced Analytics: Personalized Claim Experiences
Advanced analytics enables a new degree of personalization in claim processing. By analyzing policyholder data and preferences, insurers can customize the entire claim experience. For example, a policyholder who prefers digital communication might receive automated updates and interact via a mobile app. Someone who prefers phone calls could receive personalized support from an adjuster. This tailored approach strengthens customer relationships and boosts satisfaction. You might be interested in: Learn more about choosing the right life insurance policy.
Regulatory Shifts: Adapting to the Changing Landscape
The regulatory landscape for insurance is in constant flux. New regulations and compliance requirements emerge regularly, demanding insurers adapt swiftly. This includes staying informed about new laws, implementing robust data security, and ensuring transparent claim handling. Understanding and incorporating these changes into claim processing strategies is critical for future success.
The Human-Automation Partnership: Finding the Right Balance
While automation is transforming claim processing, human input remains vital. Machines excel at routine tasks and data analysis, allowing human adjusters to concentrate on complex claims requiring judgment, empathy, and nuanced decision-making. This collaboration optimizes efficiency and ensures policyholders receive the support they need during challenging times. This evolving partnership between automation and human expertise will continue to shape the future of claims processing. For claims leaders, understanding these evolving trends is essential for making informed decisions about technology investments and developing effective strategies for future success in the dynamic insurance landscape.
Comments are closed.